Careers In The Nicu

The Neonatal Intensive Care Unit (NICU) is a specialized healthcare setting dedicated to providing intensive care to newborn babies who require medical attention and support due to prematurity, birth complications, or various medical conditions. Working in the NICU offers a unique and rewarding career path for healthcare professionals, allowing them to make a significant impact on the lives of the smallest and most vulnerable patients.
In this article, we will explore the diverse careers available within the NICU, highlighting the roles, responsibilities, and skills required for each profession. From nurses and physicians to respiratory therapists and social workers, we will delve into the intricate world of neonatal care and the dedicated individuals who dedicate their lives to ensuring the best possible outcomes for these tiny patients.
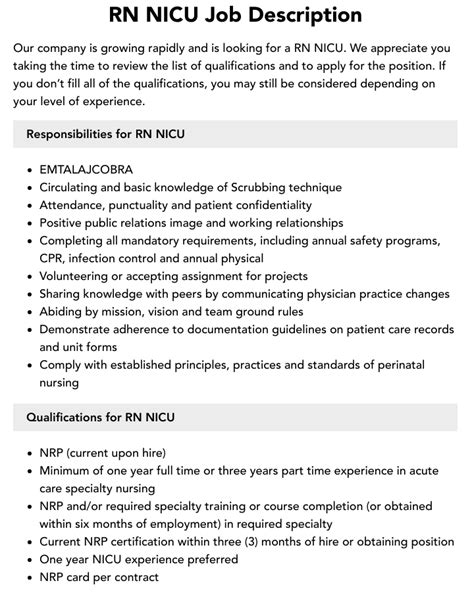
Nurses: The Cornerstone of NICU Care

Nurses are the backbone of any healthcare facility, and in the NICU, their role is absolutely vital. NICU nurses are highly skilled and trained professionals who provide round-the-clock care to newborn infants. They are often the first line of defense, monitoring and assessing the baby’s vital signs, administering medications, and providing hands-on care to meet the infant’s unique needs.
The responsibilities of a NICU nurse are extensive and demanding. They must possess exceptional clinical skills, including the ability to interpret complex medical data, recognize subtle changes in a baby's condition, and make critical decisions to ensure optimal care. NICU nurses also play a crucial role in educating and supporting parents and families, guiding them through the often challenging journey of having a baby in the NICU.
To become a NICU nurse, one typically needs to obtain a Bachelor of Science in Nursing (BSN) degree and pass the NCLEX-RN exam. Many NICU nurses also pursue additional certifications, such as the Neonatal Resuscitation Program (NRP) certification, to enhance their expertise and demonstrate their commitment to neonatal care.
Skills and Qualifications:
- Critical Thinking and Decision-Making: NICU nurses must analyze complex medical data and make quick, informed decisions to ensure the best outcomes for their patients.
- Attention to Detail: Precision and accuracy are essential when dealing with delicate medical equipment and administering medications to tiny infants.
- Communication Skills: Effective communication is crucial for coordinating care with the multidisciplinary NICU team and providing emotional support to families.
- Empathy and Compassion: The ability to empathize with families going through a difficult time and provide emotional support is a key trait of successful NICU nurses.
- Flexibility: NICU nursing requires adaptability to handle changing patient needs and unexpected situations that may arise.
| NICU Nurse | Qualifications and Certifications |
|---|---|
| BSN Degree | RN License |
| NRP Certification | Advanced Neonatal Resuscitation Training |
| Critical Care Training | Specialized NICU Courses |

Neonatologists: Leading the Medical Team

Neonatologists are highly specialized physicians who lead the medical team in the NICU. These doctors are experts in the field of neonatology, focusing on the care of newborn infants, particularly those with critical illnesses or requiring intensive medical attention.
The role of a neonatologist is multifaceted and demanding. They are responsible for diagnosing and treating a wide range of medical conditions affecting newborns, from prematurity and respiratory distress to congenital anomalies and infections. Neonatologists work closely with the NICU nursing staff, providing medical guidance, prescribing medications, and overseeing the overall medical management of their patients.
To become a neonatologist, one must complete an extensive medical education journey. After obtaining a medical degree and completing a pediatric residency, aspiring neonatologists pursue further specialization through a neonatology fellowship program. This additional training equips them with the advanced knowledge and skills required to excel in this highly specialized field.
Skills and Expertise:
- Advanced Medical Knowledge: Neonatologists possess a deep understanding of neonatal physiology, pharmacology, and the unique challenges faced by premature or sick newborns.
- Diagnostic and Clinical Skills: They are adept at interpreting medical scans, laboratory results, and vital signs to make accurate diagnoses and develop effective treatment plans.
- Critical Care Management: Neonatologists are skilled in managing complex medical conditions, often involving the use of advanced life support systems and specialized equipment.
- Leadership and Communication: As leaders of the NICU team, neonatologists must effectively communicate with colleagues, coordinate care, and provide clear guidance to the nursing staff and other healthcare professionals.
- Research and Innovation: Many neonatologists contribute to medical research, striving to advance the field and improve outcomes for newborn infants.
| Neonatologist | Education and Specialization |
|---|---|
| Medical Degree (MD or DO) | Pediatric Residency |
| Neonatology Fellowship | Advanced Neonatal Care Training |
| Board Certification in Neonatology | Research and Publications in Neonatal Medicine |
Respiratory Therapists: Breathing Life into Tiny Lungs
Respiratory therapists play a crucial role in the NICU, focusing specifically on the respiratory health of newborn infants. These healthcare professionals are experts in respiratory care, ensuring that babies with breathing difficulties receive the necessary support and treatment.
In the NICU, respiratory therapists work closely with neonatologists and nurses to manage and monitor the respiratory status of their patients. They are skilled in administering various respiratory therapies, such as oxygen therapy, mechanical ventilation, and non-invasive respiratory support techniques. Respiratory therapists also perform diagnostic procedures, such as arterial blood gas analysis, to assess the baby's oxygenation and respiratory function.
To become a respiratory therapist, individuals typically complete a respiratory therapy program at an accredited college or university. These programs provide a solid foundation in anatomy, physiology, and respiratory care, along with hands-on clinical training. Many respiratory therapists also pursue additional certifications, such as the Neonatal Pediatric Specialist (NPS) certification, to enhance their expertise in neonatal care.
Key Responsibilities and Skills:
- Respiratory Care: Administering oxygen therapy, mechanical ventilation, and other respiratory support techniques to ensure optimal breathing for infants.
- Diagnostic Assessments: Performing arterial blood gas analysis and other diagnostic tests to evaluate respiratory function and guide treatment decisions.
- Equipment Management: Maintaining and troubleshooting respiratory equipment, ensuring its proper functioning and safety.
- Collaboration: Working closely with the NICU team, including neonatologists and nurses, to coordinate respiratory care and participate in multidisciplinary rounds.
- Patient Education: Providing education and support to parents and families, empowering them to understand their baby’s respiratory condition and the care provided.
| Respiratory Therapist | Qualifications and Certifications |
|---|---|
| Respiratory Therapy Degree | Registered Respiratory Therapist (RRT) License |
| Neonatal Pediatric Specialist (NPS) Certification | Advanced Respiratory Care Training |
| Pediatric Advanced Life Support (PALS) Certification | Continuing Education in Neonatal Respiratory Care |
Social Workers: Supporting Families Through the NICU Journey
The NICU journey can be emotionally challenging for families, and that’s where social workers play a vital role. NICU social workers provide comprehensive support and guidance to families, helping them navigate the complex emotions and decisions associated with having a baby in the intensive care unit.
Social workers in the NICU are skilled in providing emotional support, counseling, and advocacy for families. They help families cope with the stress and anxiety of having a sick or premature baby, offering guidance on decision-making, coordinating community resources, and providing information on available support services. Social workers also assist with discharge planning, ensuring a smooth transition from the NICU to home or another care setting.
To become a NICU social worker, individuals typically need a master's degree in social work (MSW) and relevant experience in healthcare or social services. Many NICU social workers also pursue additional certifications, such as the Certified Child Life Specialist (CCLS) certification, to enhance their expertise in working with children and families in medical settings.
Key Responsibilities and Skills:
- Emotional Support and Counseling: Providing a listening ear, offering empathy, and helping families process their emotions during the NICU journey.
- Advocacy and Resource Coordination: Advocating for families, connecting them with community resources, and ensuring they have access to the support they need.
- Discharge Planning: Assisting with the transition from the NICU to home or another care setting, ensuring a well-coordinated and smooth discharge process.
- Communication and Collaboration: Collaborating with the multidisciplinary NICU team, including healthcare professionals and family members, to ensure a holistic approach to care.
- Cultural Competence: Understanding and respecting the diverse cultural backgrounds of families, tailoring support and resources to meet their unique needs.
| NICU Social Worker | Qualifications and Certifications |
|---|---|
| Master of Social Work (MSW) | Licensed Clinical Social Worker (LCSW) |
| Certified Child Life Specialist (CCLS) | Advanced Training in Pediatric Social Work |
| Cultural Competence Training | Discharge Planning and Transition Skills |
Lactation Consultants: Promoting Breastfeeding Success
Breastfeeding is an essential aspect of neonatal care, and lactation consultants play a crucial role in supporting and educating mothers in the NICU. These healthcare professionals are experts in lactation and breastfeeding, helping mothers navigate the challenges and rewards of breastfeeding their premature or sick infants.
In the NICU, lactation consultants provide one-on-one counseling and support to mothers, guiding them through the breastfeeding process. They offer education on the benefits of breastfeeding, assist with latching techniques, and provide practical tips for successful breastfeeding. Lactation consultants also advocate for breastfeeding rights and work closely with the NICU team to ensure a breastfeeding-friendly environment.
To become a lactation consultant, individuals typically need to complete a lactation consultant training program and pass a certification exam. These programs cover a range of topics, including breastfeeding physiology, infant nutrition, and counseling skills. Many lactation consultants also pursue additional certifications, such as the International Board Certified Lactation Consultant (IBCLC) certification, to further enhance their expertise.
Key Responsibilities and Skills:
- Breastfeeding Support and Education: Providing individualized counseling and education to mothers, helping them overcome breastfeeding challenges and achieve success.
- Latching and Positioning: Assisting mothers with proper latching techniques and positioning to ensure effective milk transfer and comfort for the baby.
- Pumping and Milk Storage: Guiding mothers on using breast pumps, storing milk safely, and maintaining milk supply while their baby is in the NICU.
- Breastfeeding Advocacy: Advocating for breastfeeding rights, promoting a breastfeeding-friendly environment within the NICU, and supporting mothers in their breastfeeding goals.
- Collaboration: Working closely with the NICU team, including nurses and physicians, to ensure a coordinated approach to breastfeeding support.
| Lactation Consultant | Qualifications and Certifications |
|---|---|
| Lactation Consultant Training Program | Certified Lactation Counselor (CLC) |
| International Board Certified Lactation Consultant (IBCLC) | Advanced Breastfeeding Support Training |
| Breastfeeding Advocacy Skills | Cultural Competence in Lactation Support |
Other Essential NICU Professionals
While nurses, neonatologists, respiratory therapists, social workers, and lactation consultants are the primary careers within the NICU, there are other essential healthcare professionals who contribute to the overall care and well-being of newborn infants.
Additional NICU Careers:
- Physiotherapists: These professionals provide physical therapy and rehabilitation to help premature or sick infants develop their motor skills and reach developmental milestones.
- Speech and Language Therapists: Speech therapists work with infants who have feeding or swallowing difficulties, helping them develop their oral motor skills and ensuring safe and effective feeding.
- Dietitians: Dietitians play a crucial role in ensuring proper nutrition for NICU infants, developing individualized feeding plans, and providing education to parents on infant nutrition.
- Nurse Practitioners: Nurse practitioners (NPs) are advanced practice nurses who provide comprehensive medical care, often serving as the primary healthcare providers for infants in the NICU.
- Pharmacy Specialists: Pharmacy specialists in the NICU ensure the safe and effective use of medications, preparing and administering medications tailored to the unique needs of newborn infants.
Conclusion: A Fulfilling Career Path
Working in the NICU offers a unique and rewarding career path for healthcare professionals who are passionate about making a difference in the lives of newborn infants and their families. From nurses and neonatologists to respiratory therapists and social workers, each career within the NICU plays a vital role in ensuring the best possible outcomes for these tiny patients.
The NICU environment is fast-paced, demanding, and emotionally challenging, but it is also incredibly rewarding. The opportunity to witness the growth and progress of these fragile infants, to see them thrive and go home with their families, is a powerful motivator for those who choose to dedicate their careers to neonatal care.
If you are considering a career in the NICU, whether as a nurse, physician, therapist, or support staff, know that your skills and dedication will make a significant impact. The NICU is a place of hope, resilience, and incredible teamwork, and your contribution will be valued and cherished by the infants and families you serve.
What are the educational requirements for a career in the NICU?
+Educational requirements vary depending on the specific career path. Nurses typically need a BSN degree and an RN license, while neonatologists require a medical degree and specialized training. Respiratory therapists often complete a respiratory therapy program, and social workers require a master’s degree in social work. Lactation consultants may need a lactation consultant training program and certification.
What skills are essential for working in the NICU?
+Essential skills for NICU careers include critical thinking, attention to detail, communication, empathy, and flexibility. NICU professionals must be able to work effectively in a fast-paced environment, collaborate with a multidisciplinary team, and provide compassionate care to infants and their families.